Have you ever had a hard time catching your breath after walking up a flight of stairs? What we once took two at a time now feels like Mount Everest! The thing is, energy loss can be attributed to natural aging — but some symptoms may also be warning signals that your heart is not functioning as well as it used to. So, is there a connection between menopause and the risk of cardiovascular disease? And how do we know if that chest pain will wear off or if it’s time to see the doctor?
In this article, I will let you understand the relationship between menopause and the risk of cardiovascular disease (CVD). You will also learn about different symptoms and poor habits that can trigger CVD risk!
Don’t worry, this is not an article that magnifies the risk of getting cardiovascular disease in menopause. I will share different ways to get ahead of CVD, and various tests you can take if you think you’re experiencing some heart problem symptoms!
Now read on and let me help you go out of the “risk lane”! ?
What Links Menopause and the Risk of Cardiovascular Disease?
Cardiovascular disease (CVD) is the leading cause of death worldwide for both men and women. Although rates have decreased because of advances in diagnosis, prevention and treatment, one in three US women still dies from heart disease — and more women than men die because of CVD.
But menopause itself does not cause cardiovascular disease.
As we age, the risk of getting cardiovascular disease increases for everyone — not only for menopausal women. Generally, many factors can “make or break” the misfortune of CVD.
Dr. Nieca Goldberg, Cardiologist and American Heart Association volunteer, said that certain risk factors (for CVD) increase around the time of menopause. If you had unhealthy habits earlier in life, like smoking and eating foods high in saturated fats, they can also take a toll on your risk of having CVD!
Neither menopause nor cardiovascular disease is a one-shot thing! So, what’s the bridge that links the two? ?
Well, there’s a fair amount of research that connects menopause with cardiovascular disease — including risk factors like increasing LDL (bad cholesterol) levels and decreasing HDL (good cholesterol) levels. Cholesterol is a waxy, fat-like substance found in every cell in your body. Additionally, “total cholesterol” refers to the total amount of cholesterol present in your blood. Your total cholesterol includes:
- Low-density lipoprotein or LDL (the “bad guy”)
- High-density lipoprotein or HDL (the “good guy”)
- Triglycerides (another form of fat in your blood that can increase CVD risk)
Women’s total cholesterol levels have been found to increase after menopause. Total cholesterol levels peak in women between 55–65 years of age — that’s about ten years later than the peak in men.
More studies also found that women with early menopause onset (45 and younger) have more cardiovascular health issues in their later years than those who had menopause closer to the normal age (around 50).
Menopause is just one of the risk factors; it is not the main villain for cardiovascular disease.
At this time in our lives, we all know that so many changes happen to our body — inside and out! For one, estrogen deficiency has a negative effect on cardiovascular function and metabolism. Estrogen is also a regulator of cholesterol levels in the body. Therefore, when estrogen levels drop, our body’s natural protective effect against CVD is lost — increasing our risk of heart-related problems!
Moreover, menopause holds many traditional CVD risk factors:
• Emotional stress: Emotions such as depression, anxiety, fear, panic and grief cause constriction in our blood vessels. Such strong emotions impede the free flow of blood. Anything that causes constriction in your blood vessels makes your heart and vessels work harder to do their job!
• Insulin resistance: Insulin resistance is present to some degree in 50% – 75% of women in the United States. Studies show that a high-carb diet with low-fat consumption is likely to increase the risk of heart disease. This is due to the ad adverse effects of this diet combination on lipids and insulin
• Changes in body fat distribution: Menopause-related changes in body fat distribution is one of the risk factors of cardiovascular and metabolic diseases during postmenopausal years.
• Reduced glucose tolerance: Research from the Nurses’ Health Study showed that women who consumed diets with a high glycemic load (an indicator that measures how rapidly a specific carbohydrate-rich food raises blood sugar) had an increased CVD risk.
• High LDL (bad cholesterol) levels: If there is too much LDL cholesterol in the blood, it can deposit in the walls of the arteries — which increases CVD risk. These deposits are known as plaque or “atheroma”, which builds up and leads to “atherosclerosis”.
• Increased blood pressure: High blood pressure (HBP) is one of the most crucial risk factors for CVD. Approximately 54% of strokes and 47% of coronary heart diseases worldwide are attributable to HBP.
• Increased sympathetic tone: Studies show that increased sympathetic tone and faster heart rates often progress to asymptomatic cardiovascular diseases. Among patients with heart failure, increased sympathetic drive and faster heart rates are linked with mortality and sudden death.
Learn more from Dr. Susan Steinbaum, the Director of Women’s Heart Health at Lenox Hill Hospital in New York City, as she explains the connection between menopause and the risk of cardiovascular disease! ?
Heart Problem Symptoms: When Do Things Become Serious?
The earliest symptoms of heart failure are often very subtle.
While it’s dangerous to ignore them, it’s fatal not to have any knowledge! Fortunately, the Heart Failure Society of America [www.HFSA.org] developed a handy tool that goes by the acronym “FACES”. This tool was made to help both doctors and patients quickly spot a possible combination of heart failure symptoms:
F = Fatigue. When the heart can’t pump enough oxygen-rich blood to meet the body’s energy needs, a general feeling of tiredness or fatigue sets in.
A = Activity limitation. People with heart failure are often unable to do their normal activities because they become easily tired and short of breath.
C = Congestion. Fluid buildup in the lungs can result in coughing, wheezing and breathing difficulty.
E = Edema or ankle swelling. When the heart doesn’t have enough pumping power to force used blood back up from the lower extremities, fluid can collect in the ankles, legs, thighs, and abdomen. Excess fluid can also cause rapid weight gain.
S = Shortness of breath. Fluid in the lungs makes it more difficult for carbon dioxide to be exchanged for fresh oxygen. It may also be harder to breathe when lying down — gravity allows fluid (below the lungs) to travel up the torso.
By themselves, these five warning signs do not confirm a diagnosis of heart failure, but they do convey a sense of urgency to seek medical advice. Moreover, the following are other early signs and symptoms of having CVD:
- Lack of appetite
- Nausea
- Confusion, impaired thinking, brain fog
- Memory loss
- Increased heart rate or palpitations
- Shortness of breath
- Persistent coughing or wheezing
- Weight gain
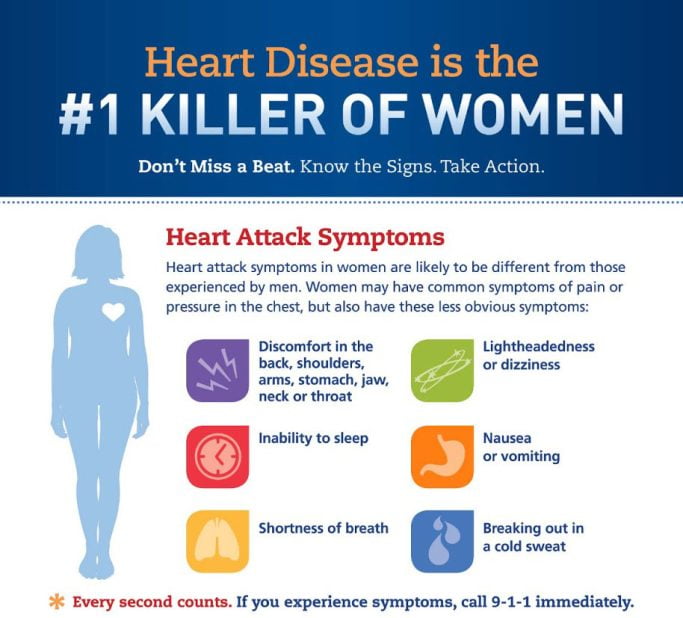
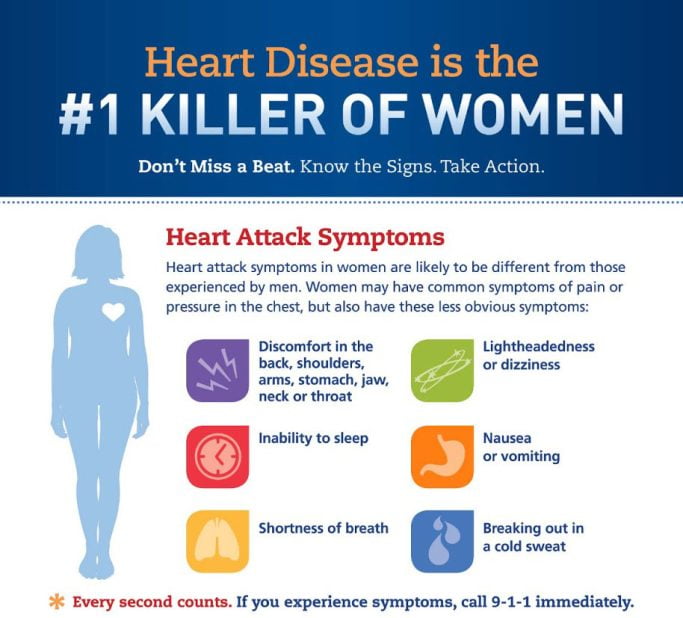
Do men and women show the same heart problem symptoms? ?
According to the American Heart Association, women have long been disadvantaged in preventing and managing cardiovascular diseases. That means, the typical symptoms of women are different from the symptoms that men show.
For years, medical practitioners have paid more attention to common symptoms in men — such as chest pain. On the other hand, women show a different set of symptoms that may have been unrecognized by conventional medical procedures. Therefore, we must be seriously aware and knowledgeable about our symptoms!
Generally, cardiovascular disease (CVD) is any condition that involves a malfunction in the heart (cardio) or blood vessels (vascular). Among the most rampant cases of CVDs are:
- Coronary Heart Disease – when the arteries of the heart cannot deliver enough oxygen-rich blood anymore to the heart
- Cerebrovascular Disease – a condition that affects the flow of blood to the brain
- Peripheral Arterial Disease – narrowing of arteries resulting in reduced blood flow to the head, arms, stomach and legs
- Congenital Heart Disease – a birth defect that affects the normal development and functioning of the heart
- Rheumatic Heart Disease – when the heart valves are damaged permanently due to rheumatic fever, a condition caused by streptococcal infection; repeated strep infections can cause the immune system to react against the tissues of the body — inflaming and scarring the heart valves
- Deep Vein Thrombosis – when a blood clot develops in the deep veins, most commonly in the lower extremities
- Pulmonary Embolism – when a part of the blot clot in the veins breaks off, then travels to the heart and lungs
Lifestyle Factors: What Habits Can Trigger Cardiovascular Problems?
Besides the traditional CVD risk factors we tackled, poor lifestyle habits can also harm cardiovascular health. So, if ever you’re still guilty of any of the things below, shake these bad habits off now, sweetie! ?
- Sedentary Lifestyle: Evidence demonstrates a strong association between the amount of physical activity and cardiovascular mortality.
- Cigarette Smoking: Smoking is responsible for 55% of cardiovascular deaths in women less than 65 years old. Smoking significantly increases oxidative stress in every cell of the body! The Nurses’ Health Study showed that smokers had a four times higher risk of total coronary artery disease than non-smokers.
- Poor Diet: A study by the Netherlands Epidemiology of Obesity showed that dietary intake of fruits, vegetables, plant-based fats and oils was associated with less visceral fat. Intake of sweet snacks was associated with more liver fat. These unhealthy fats can cause plaque along the blood vessels. More than half of the women in the study were postmenopausal.
- Insufficient and Poor Sleep Quality: Sleep disturbance, a common symptom during menopause, is linked to a greater risk of CVD in midlife women. Watch this video from Dr. Rebecca Thurston as she discussed the relationship between sleep and cardiovascular disease in menopause patients. She presented this research during the North American Menopause Society (NAMS) 27th Annual Meeting! ?
How Can I Prevent Cardiovascular Disease in Menopause?
1. Let Food Be Thy Medicine!
To ensure optimal cardiovascular health, it is important to know the best heart-healthy foods! Go for healthy fats, fish, shellfish, lots of veggies, grass-fed meat and plant-based proteins! They are abundant in the Mediterranean diet and Keto-Green way of eating. Below are healthy food choices to keep your cardiovascular health in tiptop condition:
- Fish (high in omega-3 fatty acids: salmon, tuna, mackerel, herring and trout)
- Healthy nuts: almonds, walnuts, cashew, pistachio, chestnut, hazelnut
- Berries are chock full of heart-healthy phytonutrients and soluble fiber
- Seeds (rich in omega-3 fatty acids, fiber, protein and phytoestrogens: flaxseeds, chia seeds, sunflower seeds, pumpkin seeds)
- Legumes (high in fiber, B-vitamins and minerals: dried beans, lentils, garbanzo, pinto, kidney beans or black beans
- Green veggies: spinach, kale, Swiss chard, collard/mustard greens, bok choy, broccoli, asparagus, arugula
- Dark chocolate (the higher the percentage of cocoa the better!)
- Avocados (rich in heart-healthy monounsaturated fats)
- Fresh herbs: hawthorn, garlic, turmeric, motherwort, basil, cilantro
- Plant-based oils: olive oil, avocado oil, nut/seed oils
- Shellfish
- Eggs
- Lean poultry
- Pomegranate (rich in flavonoids that can prevent the development of atherosclerotic disease)
2. Supplement!
Vitamins and supplements are proven to be your heart’s best buddies! If you have a condition that may be stopping you from getting enough nutrients from your diet, studies recommend taking:
- Coenzyme Q10
- Omega-3 fatty acids
- Vitamin K
- L-Carnitine
- D-Ribose
- Magnesium
- Potassium
- Vitamin E
- Vitamin D
- Green tea extract
3. Exercise!
How much can exercise do for our cardiovascular health? ?
- Boosts “good cholesterol” levels
- Strengthens your heart muscle
- Improves your body’s ability to use oxygen
- Helps you maintain a healthy weight
- Increases your parasympathetic nervous system (rest and digest) response
- Reduces your risk of type 2 diabetes
- Lowers stress
- Makes you feel happier!
Include weight-bearing exercises in your daily routine! These exercises are beneficial for heart health because they lower insulin resistance and increase lean muscle. And because lean muscle mass has a higher metabolic rate than fat, it helps burn excess body fat and, in turn, reduces the risk of heart disease!
Women who perform such exercises live an average of 6 years longer than those who do not. The best fitness regimen includes strength, flexibility and endurance, so choose activities that cover each of these!
4. Get Tested!
• Heart scan, also known as a “coronary calcium scan”, is a specialized X-ray test that provides pictures of your heart that can help your doctor detect and measure calcium-containing plaque in your arteries.
• Echocardiogram (often called an “echo”) is a simple, non-invasive test that uses ultrasound to create images of your heart while it beats. If the echo shows a lower-than-normal percentage of blood leaving the heart, there is a strong possibility of heart muscle damage. Other findings that point to heart failure include abnormal thickening and ballooning of the heart wall and malfunctioning heart valves.
Doctors also look for biomarkers in the blood, which are released when the heart is under stress. “I call these compounds ‘tears from the heart’ because they show that the heart is crying for help,” says Dr. Mehra.
Once the initial diagnosis is confirmed, further testing may be needed to determine what’s causing the heart’s dysfunction and determine the best treatment approach!
Now, I think it’s about time to know how heart problem symptoms differ between men and women. Here’s an interview video from Scripps Health cardiologists, Dr. Poulina Uddin and Christina Adams! ?
Takeaway
Well, that’s a wrap! I hope you’ve learned the factors that link menopause and the risk of cardiovascular disease (CVD)! I also discussed some bad habits that trigger the risk of cardiovascular problems. Don’t forget about the heart problem symptoms to watch out for!
Above all, embrace different ways to get ahead of CVD. Now, you can make your way out of the “risk lane”! Take menopause as your time to take care of your body, honey.
Fill your heart with peace, love and laughter! ?
Fact Box
• Primordial Prevention: The Best Kind in Preventing Heart Disease
The word “primordial” means existing from the beginning. Primordial prevention involves working to prevent inflammation, atherosclerosis and endothelial dysfunction from taking hold! Thus, it prevents risk factors such as high blood pressure, high cholesterol, excess weight and ultimately cardiovascular events. Once rarely discussed, primordial prevention is now the cornerstone of the American Heart Association’s definition of ideal heart health and efforts to help people achieve it. As its name implies, the sooner you can start practicing primordial prevention, the more likely you are to achieve it and protect yourself from heart disease!
• How Do Heart Attacks and Strokes Happen?
Atherosclerosis is a condition that develops when “plaque” builds up in the walls of the arteries. This plaque is made up of “bad cholesterol” or fatty deposits. It narrows our arteries and makes it harder for blood to flow through. If a blood clot forms out of the “growing” plaque, it can block the blood flow — resulting in a heart attack or stroke.
To give you a visual explanation of how plaque builds up, watch this video from Dr. Paul Zollinger-Read of Bupa Health UK! He also briefly discussed the factors that cause atherosclerosis and heart-related problems! ?
• Hormone Replacement Therapy Timing
Observational studies and randomized clinical trials suggest that menopausal hormone therapy (MHT) started soon after menopause can provide cardiovascular benefits. Hormone replacement therapy (HRT) and bioidentical hormone replacement therapy (BHRT) are the different forms of MHT.
In 2006, an analysis from the Nurses’ Health Study data found that nurses who began taking HRT near menopause, had about 30% lower risk for heart disease than women who didn’t take HRT. In comparison, nurses who started HRT 10 years or more after menopause showed no benefit. There was no difference between those who took estrogen alone and those who took it combined with synthetic progestin.
Discover the differences between HRT and BHRT in my article! You will also learn more ways to prevent possible risks and maximize the benefits! ?
• Statins: What Are They and How “Safe” Are They?
Statin drugs are prescribed to lower cholesterol and prevent heart problems. The myth is that lowering bad cholesterol is the only key to preventing heart disease. But recent studies say that things are beyond that. Studies show that statins deplete the body’s CoEnzyme Q10 (CoQ10) — a vital nutrient for producing energy in the cells. Of all the organs, the heart requires the most energy. CoQ10 is a vital nutrient that helps make sure that the heart functions optimally. It is also shown to support the heart as well as every cell in the body!
“While I believe in the body’s ability to heal itself in most instances, there are times when you absolutely need medication to treat bothersome symptoms or to decrease the chance of an illness progressing. When this is the case, I recommend choosing the safest medications with the fewest number of side effects whenever possible.” — Dr. Christiane Northrup
• What You Need to Know About “Safe Drugs”
According to Women’s Health expert Dr. Christiane Northrup, each drug that you are prescribed or can purchase over-the-counter goes through randomized controlled trials to determine its benefits. The measurement used to determine treatment benefits is called the “number needed to treat” (NNT).
Number Needed to Treat (NNT): NNT refers to the number of patients who need to be treated in order to prevent one bad outcome (like heart attack or stroke). So, if a drug has an NNT of 10, it means you have to treat 10 people with the drug to prevent one person from having a bad outcome. The ideal NNT is 1 — which means every patient who is treated will benefit.
Number Needed to Harm (NNH): NNH indicates how many patients need to be exposed to a risk factor for it to cause harm to one patient (who would not have been harmed). To give you a picture, a comprehensive study on statins given to people with no known heart disease shows why you need to be aware of the NNT and NNH for any drug.
Over 5 years, only 1 in 104 patients had a heart attack prevented, and only 1 in 154 had a stroke prevented. The same study showed that 1 in 100 was harmed because they developed diabetes as a direct result of statins, and 1 in 10 developed muscle damage! To sum up, the lower the NNH of the drug, the worse the risk factor.
“The report on statins also summarizes that the risk of harm may still be underestimated, and that diet and lifestyle interventions are substantially more powerful than medication in protecting your heart and preventing heart attack and stroke — something I have been saying for decades!” — Dr. Christiane Northrup
• Can Panic Attacks Lead to Heart Attacks?
A panic attack is a sudden feeling of overwhelming fear or anxiety. It is not life-threatening, but can interfere with your quality of life and mental well-being! According to Dr. Mistyann-Blue Miller of the Cleveland Clinic, a panic attack is unlikely to cause a heart attack, but it’s possible. Emotional stress plays a crucial role in both conditions! Both panic attacks and heart attacks can occur during or after a stressful situation, but most of the time, women experience a panic attack (rather than a heart attack) in response to emotional stress.
Knowing the difference between a panic attack and a heart attack can be difficult, especially for a woman who has never experienced the symptoms of either before. Chest pain is common to both conditions, but the characteristics of the pain often differ. Experts say that the pain of a heart attack extends to other areas like the arm, jaw or neck. On the other hand, the pain of a panic attack typically stays in the chest.
Learn how to manage panic attacks in my article here!


We would love to hear your thoughts so feel free to add your comments below
Let´s support each other. Use the share buttons in this article, so more women can get help and feel great!
References:
pubmed.ncbi.nlm.nih.gov/13679667/
pubmed.ncbi.nlm.nih.gov/23041081/
heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/menopause-and-heart-disease
hopkinsmedicine.org/health/conditions-and-diseases/menopause-and-the-cardiovascular-system
pubmed.ncbi.nlm.nih.gov/17364594/
heart.org/en/health-topics/heart-failure/warning-signs-of-heart-failure
ahajournals.org/doi/10.1161/CIR.0000000000000912
bhf.org.uk/informationsupport/support/women-with-a-heart-condition/menopause-and-heart-disease
health.harvard.edu/heart-health/5-warning-signs-of-early-heart-failure
mayoclinic.org/tests-procedures/heart-scan/about/pac-20384686
thefhfoundation.org/do-you-know-the-early-signs-of-heart-disease
drnorthrup.com/heart-disease/
drnorthrup.com/cholesterol-doesnt-always-count/
thennt.com/nnt/statins-for-heart-disease-prevention-without-prior-heart-disease-2/
drnorthrup.com/three-drugs-that-i-would-not-take/
pubmed.ncbi.nlm.nih.gov/14695925/
clinicalkey.com/#!/content/book/3-s2.0-B9780702072994000327
health.clevelandclinic.org/the-difference-between-panic-attacks-and-heart-attacks/
👉 What to Do Next
Don’t go just yet — especially if you’ve been feeling off and no one’s given you real answers.
Go to the START HERE page.
It’s where things begin to feel clearer. No more second-guessing, no more sorting through conflicting advice. Just calm, honest support for where you are right now.
And if you haven’t yet, download the FREE GUIDE.
It’s quick, clear, and made to help you feel better — without having to turn your whole life upside down.


Gita is the founder of My Menopause Journey. Since 2014, she has been supporting midlife women by sharing hard-earned learnings from her own experience. To advance her knowledge, Gita puts a lot of her time and effort into understanding the broad spectrum of women’s health. She immerses in extensive research about the physical, mental and emotional aspects of menopause. Gita believes in the life-changing power of healthy, holistic living — this is where she anchors her message to all women. Learn more about her marvelous mission in About us - My Menopause Journey.