Our bones, though we may not notice it, go through a lot of changes. Old bones are lost and replaced by new ones as we grow older. During menopause and as we continue to age, we lose more bones faster than we can rebuild.
Is this something we should worry about?
Well, to start, bone loss is a natural part of aging. Not to mention how the miracles of modern medicine and public health initiatives have indeed helped us live longer than we did decades ago. This fact goes a sad reality that losing bone mass has become more of a problem nowadays.
However, getting a tiny broken bone may not sound so serious when you are healthy and strong. But when you have osteoporosis, even a supposedly minor fracture can put your life on a halt.
It can disrupt your daily activities and impact your health and happiness. Even the simplest task of walking can become a struggle.
Osteoporosis is not a normal part of growing older. You should not experience painful broken bones. You should be grooving, swaying and dancing instead!
So, here we will talk about the different osteoporosis treatments and remedies. However, it is best if we first learn about the causes and risks of osteoporosis.
What is osteoporosis?
Literally, osteoporosis means “porous bones”. It is a condition where our bones become thin and lose their strength. As a result, they become fragile and prone to fracture. Even a minor bump could crack your bone easily when you have osteoporosis.
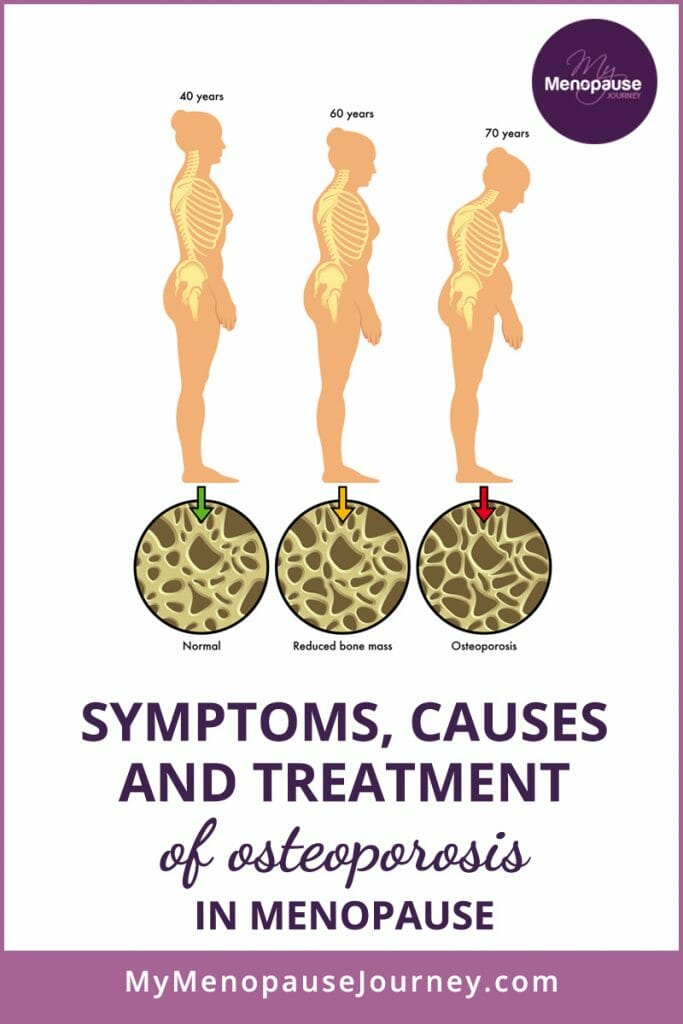
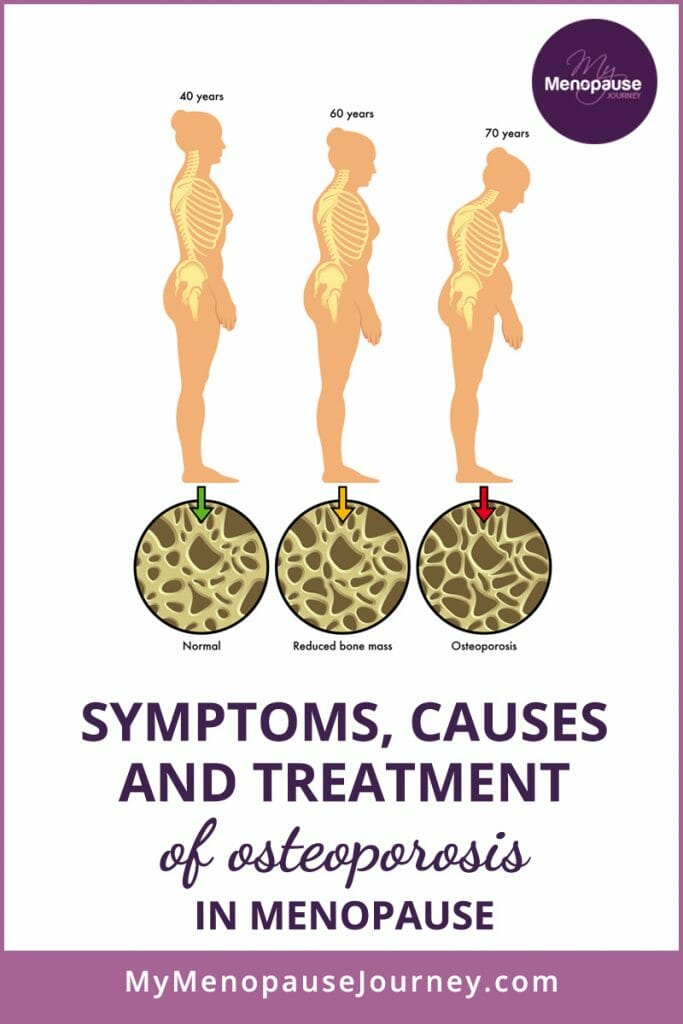
If you look at a healthy bone under the microscope, it appears like a honeycomb. When osteoporosis occurs, the honeycomb’s holes and spaces are much larger compared to a healthy bone. Your bones also lose their density and have abnormal tissue structures. As bones become less dense, they weaken and then break more easily.


Our bones are living tissues, and therefore, are constantly changing. They have their own blood vessels and are made of living cells, which help them grow and repair themselves.
Proteins, minerals and vitamins also make up the bones. When we are young, our body makes new bones faster than it breaks down old ones. As a result, our bone mass increases. By the time we reach the “peak bone mass”, things start to slow down.
Bone loss normally starts in our 30s and increases rapidly five to ten years after menopause. Men, on the other hand, begin losing bones slowly in their 50s and experience rapid bone loss in their 70s.
The amount of bone mass we have developed in our younger years can affect our bone health later in life. The higher the peak bone mass we have, the more bones we have “in the bank”. This lowers our chances of getting osteoporosis as we age.
Bone loss happens without any warning signs, which is why osteoporosis is called a “silent disease.” Depending on its root cause, osteoporosis comes in two forms:
1.) Primary osteoporosis: This is due to aging, menopause and unhealthy lifestyle practices such as smoking, calcium and vitamin D deficiency, and sedentary lifestyle.
2.) Secondary osteoporosis: This is caused by low bone mass and changes in the detailed structure of the bones, leading to fragility fractures. This form of osteoporosis happens in the presence of an underlying disease or medication.
How does estrogen affect osteoporosis and what makes women in menopause at high risk?
In menopause, estrogen deficiency (ED) leads to a damaged “cortical bone” – the dense outer surface of the bone that forms a protective layer. ED also induces spongy bones, also known as “cancellous bone.” This leads to faster degradation of the skeleton. Within the first ten years after the onset of menopause, as much as 25% of our bone mass can disappear. After this, the decline in bone mass returns to a more normal rate.
For women who experienced menopause before the age of 45, or had a removal of ovaries (hysterectomy), the risk of developing osteoporosis goes up. The primary reason for this is because ovaries produce estrogen, and when estrogen drops way earlier than it should, it then results to faster bone loss.
What causes osteoporosis and what happens to the bones during menopause?
As estrogen and progesterone levels begin to fall when women reach the menopausal mark, these hormonal deficiencies then lead to the development of osteoporosis.
But bear in mind that decreased hormonal levels are just one of the causes of osteoporosis. Several factors may be responsible for weakened bones too! When these factors are combined with menopause, osteoporosis may begin or develop faster.
Remember that all of us are directly, though unknowingly, responsible for ourselves. So let’s get to know these factors and be saved from the pain of not knowing, and the pain of osteoporosis!
Lack of Vital Nutrients
Calcium is a mineral that always goes along when we talk about bone health. But I might leave you in a slight surprise if I told you that it’s not the “lacking” of calcium that always leads to weaker bones, but the “malabsorption” of calcium. It’s either too little calcium is absorbed by the gut, or the skeleton absorbs too little calcium! And since overall bone health is dependent on calcium metabolism and utilization, it means that other minerals are involved in the overall strength of our bones.
For instance, vitamin D regulates calcium uptake from food while vitamin K2 takes the calcium and deposits it to where it is needed most (bones and teeth). We usually do not have a deficiency of vitamin K. Instead, it is a deficiency of vitamin K2, vitamin D3 and magnesium that cause calcium malabsorption.
In addition, when calcium is paired with magnesium, the power of this combination helps slow down aging! Depending on their ratio, they can affect osteoporosis, blood pressure, heart diseases, depression and anxiety. The key is to have the right balance between the two! The ideal ratio of calcium to magnesium is thought to be 1:1 to 2:1. So if you’re getting say 800 mg calcium, you’d need 400 – 800 mg magnesium. Most people’s ratio is 5:1 or higher, and that’s a major problem over the long term.
Watch as Dr. Berg shares the different health problems that you can experience when you have too much calcium in the body. Learn the remedies to regulate calcium levels. [9:13]
DISCOVER MORE: After listening to Morley Robbins, the founder of “The Root Cause Protocol”, I have changed my supplement routine and started following his RCP protocol. He recommends magnesium, cod liver oil, boron and trace minerals. Apparently, these vital nutrients aren’t normally as famous as calcium, when we talk about bone strength. But after listening to Robbins, I got to learn that these “underdog” minerals actually help A LOT, not only for our bones, but for our overall health!
Physical Inactivity
We defend ourselves against osteoporosis when we exercise. Physical activities strengthen muscles and build healthy bones. Strong muscles provide stability and protect the bones from injury. At the same time, they improve our balance and coordination.
Don’t forget: your bones are alive! They change depending on the force you place upon them. When you exercise regularly, they build more cells and become denser. On the other hand, sitting constantly makes your bones grow weaker by the day. When your bones are weak, you become more susceptible to fractures.
Alcohol and Smoking
Too much alcohol in the body can negatively affect your bone health. First, alcohol puts your calcium level out of balance. Second, it blocks the liver from activating vitamin D which is essential for bone strength. Third, when you drink excessive alcohol, your cortisol levels rise. Cortisol, as a stress hormone, is known to reduce bone formation and enhance bone breakdown.
Smoking is obviously bad too. Chemicals found in cigarettes can damage the cells and organs responsible for our bone health. They also make it harder for the body to absorb calcium.
Another not-so-fun fact about cigarettes: they drive our estrogen crazy! This can lead to early menopause, especially for those women who’ve been smoking for quite a long time.
Do I have osteoporosis?
Osteoporosis doesn’t happen in a snap of a finger. It sneaks up on you slowly. The problem is that it’s very hard to know if our bones are healthy or not.
We can’t see them like we see if something’s wrong with our skin. We can’t hear it like the uneven beat of our hearts.
Those who suffer from osteoporosis didn’t know they had it until they broke a bone. Breaks often occur in the wrist, hip and spinal vertebrae.
If it occurs in the spine, you may notice that you are getting shorter as your upper back curves forward. You may also have a hard time fitting in your clothes and may experience back pain.
In worse cases, even a cough or sneeze can break your bone. Other early signs of osteoporosis are:
Receding gums – Our teeth are connected to the jawbone. If our jawbone is tearing down, our gums will move back from its original position.
Low handgrip strength – A study, titled “The Relationship of Hand Grip Strength with Bone Mineral Density and Vitamin D in Postmenopausal Women”, shows that: “Postmenopausal women with osteoporosis had lower handgrip strength than postmenopausal women with normal bone mineral density. It was also found that handgrip strength was significantly correlated with bone mineral density, but not with vitamin D in the selected study population. The patients should be encouraged to increase muscle strength for the risk management of osteoporosis in postmenopausal women.”
Weak and brittle fingernails – Nail health is a good indicator of bone health. However, other factors should also be considered, such as long-term experience in gardening and exposure of your hands to harsh chemicals.
Cramps and muscle aches – Lack of calcium, magnesium and potassium in your diet could cause leg cramps at night, while a deficiency in vitamin D can contribute to muscle pains.
Decreased overall fitness – Osteoporosis has been linked to an overall decline in physical activity. This is because you have low aerobic capacity, reduced muscle strength and problems with your balance.
Hey, I’m not here to scare you. In fact, I am here to say that we CAN fight osteoporosis together! There are several osteoporosis treatments out there to help us prevent our bones from breaking.
How can I prevent osteoporosis during menopause?
I know that some things – like genes, age and sex – can play a role. But that doesn’t mean we can’t put a stop to osteoporosis. Medical experts say osteoporosis was unheard of hundreds of years ago, but because of our modern lifestyle, it has slowly crept into our lives.
Preventing this disease should preferably have started when we were younger, but it’s not yet too late to take care of our bones. Fortunately, there are several osteoporosis treatments and remedies we can follow to protect us against this silent disease.
7 Osteoporosis Treatments and Preventions
With all this information, the question now is: “Can you rebuild bone density?” We’ll tell you how!
Try exercises for your bones
Weight-bearing exercises such as walking, jogging and climbing stairs are the easiest ways to make your bones strong. They force your body to work against gravity as you move. That encourages your body to make new bones in the process.
If you’re looking for some one-on-one guidance, here’s Ask Doctor Jo showing a few weight-bearing and muscle-strengthening exercises. These movements are targeted specifically for people with osteoporosis. [5:25]
Dancing, yoga and Tai-Chi are perfect too. Even simple movements can do wonders for your bone health. When shopping for food, lift canned goods or bags of groceries. Lift your grandchildren or some free weights. Exercising with resistance bands also gives your bones and muscles a good challenge, without putting pressure on your joints.
Physical therapist Michelle Kenway shows us a few osteoporosis workouts for strengthening the abdominal and spinal muscles. These routines are perfect for beginners. Check out her video here [6:28]:
Exercise not only maintains bone strength but also improves flexibility, balance and coordination. This then reduces your risk of falling. When you’re just starting out, make your progress slowly. Always listen to your body.
Yes, lifting weights is beneficial for weak bones. However, if you’re a newbie, you might overdo it and end up hurting yourself. If you’re not sure how to lift weights properly, you can always seek help. There’s no shame in asking!
Margaret Martin, who’s also a physical therapist, has lots of great osteoporosis exercises too. You can find all her videos here.
Wanna unleash the child in you and do a workout activity that is purely fun and beneficial? I got one word for that: Rebounders. Since my sister was diagnosed with osteoporosis, I was compelled to do some preventive measures for myself too and bought a rebounder. Oh dear, it is truly super fun to use and seeing the results, it indeed helps with my bones, balance, lymph, strength and heart!
Studies show that it has great benefits, and if you wish to know more, here’s some more info and tips to finally convince yourself to get one!
Eat a balanced diet that increases bone density
How can I increase my bone density without medication? A good diet is one of the keys.
Fill your plate with lots of vegetables like kale, broccoli, cabbage, collard, Brussel sprouts or even canned vegetables, since they have more calcium! Nuts, eggs and fish, especially sardines and salmon, are also rich calcium sources. If you think you have calcium deficiency, avoid spinach because it contains oxalates, which prevents the body from absorbing calcium.
Try adding more healthy fats in your diet too. Olive oil, avocado, eggs, fish oil, nuts and flaxseeds are good sources, and these are rich in vitamin E as well.
Magnesium is found in whole wheat, quinoa, most nuts, black beans, edamame, tofu, cultured yogurt, avocado and – you’ll like this one – dark chocolate, while collagen is found in meat, fish, bone broth and spirulina.
Vitamin K2 can be found in grass-fed animal products because animals eat vitamin K1 from plant sources, and their bodies convert it to K2, retained in their fat. Common sources are fermented products like some cheeses (Gouda and Edam).
If you’re vegan, don’t worry. K2 can also be found in natto and sauerkraut. Natto does not contain K2, but the bacteria that ferments it does. In other words, vitamin K2 found in natto isn’t natural but formed during the process of fermentation.
What about milk? You might think that milk and dairy are the best sources of calcium, but the truth is – they are not. Today’s milk is considered processed food.
Milking cows are injected with antibiotics and other chemicals to increase their production of milk. These chemicals can increase our insulin levels and are found to acidify our body’s pH, affect protein breakdown and trigger intolerance.
Did you know that Nordic countries drink the most milk in the world and yet they have the highest rate of osteoporosis? Likewise, plenty of studies have proven that hip fractures are most likely to happen to women who drink lots of milk.
This is our answer to your inquiry about which foods increase bone density. ? More information is in the Fact Box below.
Get some sun
Your osteoporosis treatment plan is not complete without the sun. Whether it’s sunny or cloudy, spending a little time outdoors every day helps your hormones in many ways. It tells the brain that we are awake, stimulating the production of serotonin.
Besides boosting our mood, serotonin enhances bone formation and reduces bone loss. At the same time, getting a good dose of daily sunshine boosts our melatonin levels at night. This means being out in daylight regulates our sleep and wake rhythm.
The cells that affect sleep hormones are mainly in the eyes, so it’s important not to wear sunglasses all the time, especially if we’re getting some safe amount of brightness from the sun, like during sunrise and sunset! You want your arms to get some sunlight as well during these beautiful moments to synthesize vitamin D better. Remember that even if the sun is not shining as brightly, it can still nourish you with vitamin D. As much as possible, avoid using sunscreen since it blocks the absorption of vitamin D and contains a lot of chemicals. None of us wants to get our skin burnt, of course, so shade yourself with a hat or enjoy some safe dose of sunlight in thin clothes!
Practice healthy habits
Healthy habits make healthy bones! Get rid of sodas, colas and energy drinks – they don’t do your body any good. Besides harming your bones, they can cause insulin resistance and diabetes because of their high sugar content. Research found that people with elevated blood sugar levels are prone to developing osteoporosis later in life.
Cut back on coffee and quit smoking, too! In the end, too much of everything (especially these chemical-ridden substances) is bad for you.
Alkalize your body
Are you in an extreme and constant acidic condition? An alkaline diet is the key. When your blood is too acid, the body will try to draw calcium out of the bones to counteract the acidity. This process explains why many people today suffer from weak bones or osteoporosis. Alkalizing is highly beneficial as it helps neutralize excess acid in the body and regulate pH levels. Thankfully, an Alkaline diet improves bone health by increasing calcium retention and activating the IGF-1 hormone, which stimulates muscle and bone repair.
A good way to alkalize the body is by drinking lemon water in the morning. You may also mix apple cider vinegar in water and drink it before meals. Both lemon and apple cider vinegar help balance your stomach’s pH level, allowing your stomach to take up calcium better.
Do Breathing Exercises
Ayurveda and traditional Chinese medicine considered breathing as crucial to health. Both even developed distinct breathing exercises for efficient air energy intake. Westerners have just discovered how deep nasal breathing can help with increasing oxygen availability for the tissues, reducing blood pressure, minimizing confusion, fear, anger, depression or anxiety and improving sleep.
The technique “bone breathing” or “bone marrow breathing” adapted in qigong (a Chinese physical exercise related to tai chi) and yoga is done by performing cautious and deep nasal breathing while concentrating on various parts of the skeleton.
Studies have shown that women practicing qigong and yoga have increased bone density. Other positive effects that relate to bone health include better mood, heart function and blood glucose regulation.
Be Watchful with The Drugs You Take
Drugs are created to treat symptoms as opposed to the root cause of the condition. If you only suppress your symptoms, instead of also addressing the very cause, your body will often protest by developing some so-called “side effects” to the medication — or even by developing another disease or complication.
There are tons of the popular drugs frequently prescribed to women that have significant side effects without the innate power to outweigh the risks. One of those are “bisphosphonates.”
You are supposed to stop taking these drugs after 3-5 years and have a break. Why is that? Too many side effects?
These popular drugs work by delaying “osteoclasts”, or the cells responsible for breaking down the bone, and enabling the “osteoblasts” or the cells that build up the bone to function more effectively, thus decelerating bone loss. That sounds like a good idea until you realize that these drugs interfere with our bodies’ natural breakdown and restoration cycle. The result is older, porous, brittle bone — and brittle bone means an increased likelihood of fractures.
My sister, diagnosed with osteoporosis, is one of those who have turned their backs on bisphosphonates after experiencing its long-term side effects. Instead, she discovered a “new” kind of exercise that works for her, even at her current age of 63! This exercise is called Osteogenic Loading.
One of today’s most fast-growing communities for Osteogenic Loading is OsteoStrong®.
OsteoStrong® is a biohack that helps you strengthen the foundation of your body – the skeletal system. Unlike other health solutions, you don’t have to spend hours at a gym or exert physical energy that will leave you feeling tired by the time you’re done. You show up as you are and OsteoStrong® handles the rest. It works for people at all ages and levels of activity to promote skeletal strength which impacts the entire body in many ways!
And if you’re ever wondering what makes up OsteoStrong®’s “biohack,” here are its features that are making it utterly successful:
• Sweat-free
• Painless
• Fast: less than 10 minutes
• Will not leave you feeling fatigued
• Will not leave you feeling sore the next day
• Once per week
Oh, did I hear your mind wondering where this OsteoStrong® could be? Do yourself a favor by checking out the OsteoStrong® nearest you and grab a free session!
Link: https://osteostrong.me/locations/
Another living testimony for this is Dr. Keith McCormick, a chiropractic doctor and a former Olympic athlete diagnosed with severe osteoporosis at 45 years old. He did not want to take bisphosphonates anymore after first experienced its bad effects in the longer run. Instead, he treated himself from a functional and integrative perspective. He is now an advocate of a “Whole-Body Approach to Osteoporosis,” which distills these complex strategies into a holistic whole-body plan to improve bone strength and overall vitality dramatically.
You can listen to him about what he did in this podcast:
Balance your hormones
The last osteoporosis treatment (but not the least) is to keep our female hormones in check. When one hormone is out of whack or a certain nutrient is missing, it creates a chain reaction throughout our whole body.
So how do you achieve hormone balance? Well, most of the tips I have shared will greatly help. But if you want to take steps further, you can try menopausal hormone therapy (HRT + BHRT).
Many doctors recommend this type of treatment to ease menopausal symptoms. Hormone therapy is also used to treat other disorders caused by declining levels of estrogen and progesterone – one of which is bone loss.
You can find more information about this osteoporosis treatment through the International Osteoporosis Foundation.
Can you undergo osteoporosis treatment regardless of you age?
To diagnose osteoporosis and determine your need for osteoporosis treatment, your doctor will perform a bone mineral density scan. This test uses a type of X-ray known as dual-energy X-ray absorptiometry (DEXA).
DEXA measures how thick or dense your bones are. It also examines how much calcium and minerals are in your bones. The results from this test will tell how likely you are to break a bone and how well your body will respond to the osteoporosis treatment.
However, the bone density scan isn’t right for everyone. The National Osteoporosis Foundation (NOF) only recommends DEXA if:
- You are a woman age 65 or older (for men, they should be 70 or older)
- You are menopausal with risk factors
- You break a bone after age 50
Other Factors that Could Contribute to Osteoporosis
Being female: Women are more vulnerable to osteoporosis than men due to menopause. We also have smaller, lighter bones than men.
Being older: Both men and women increase their risk of osteoporosis after the mid-30s. This is especially true for post-menopausal women.
Family history: Does anyone in your family have osteoporosis? Be on the lookout, as this silent thief can run in the family.
Small-boned, thin-framed: This body type tends to have less bone mass to draw from.
Being underweight: Low body weight due to malnourishment is associated with low bone mineral density and muscle weakness.
Fracture history: If you are over 50 with a history of fracture from a minor injury, you are more likely to be diagnosed with osteoporosis.
FACT BOX
Here are the nutrients that help build healthy and strong bones:
Vitamin D
This sunshine vitamin goes hand in hand with calcium. It keeps your bone strong by helping your body take up calcium. Calcium cannot build bones efficiently without vitamin D. Even if you’re taking enough calcium, either through supplements or real foods, it could go to waste if you don’t have enough vitamin D.
Collagen
The primary building block of strong bones is protein, and 90% of the bone matrix proteins consist of collagen. Collagen partners with calcium to give our bones the strength to withstand physical stress. The combination of collagen and calcium is also what makes our skeletal framework sturdy yet flexible. Dr. Anna Cabeca, a huge collagen fan herself, shares the reasons why collagen is crucial to our health as we age. In this video, she invited Lillian Zhao, the founder of Further Foods – a company that believes in natural foods’ power. Lillian explains the benefits of collagen to our bones, joints, gut, skin and many more. Watch the video here: [25:58]
Vitamin K2
We don’t often hear about this amazing vitamin, but vitamin K2 can do so much for our bone health. It takes calcium from the wrong places (e.g., arteries) and puts calcium where it belongs. It works like glue that binds calcium onto the skeleton. If you lack vitamin K2 in your diet, the calcium goes into your soft tissue, like in your kidneys and arteries. That damages your kidneys and heart over time. In Japan, vitamin K2 is often used to treat osteoporosis.
Vitamin E
Oxidative stress contributes to osteoporosis by speeding up the activity of osteoclasts. Since our body’s antioxidant defense system goes down as we hit the postmenopausal stage, we become more vulnerable to bone fractures. With vitamin E’s powerful antioxidant properties, our bone cells are protected against fast breakdown caused by oxidative stress.
Vitamin C
Similar to vitamin E, vitamin C also has antioxidant properties that protect our bone cells against oxidative stress. Besides this, vitamin C helps in the formation of collagen, enhances calcium absorption and increases the effect of vitamin D on bone metabolism.
Magnesium
Various processes in our body require enzymes – small proteins that build up, break down and transport materials in the body. Most of the body’s enzymes need magnesium. Magnesium is one of the most abundant minerals in our body and is part of many biochemical reactions. When it comes to bone health, magnesium helps in the absorption and metabolism of calcium and vitamin D, making it important for bone formation. Much of the body’s magnesium is found in bone tissue. Studies show that adequate levels of magnesium increase bone mineral density. This lowers the risk of bone fractures and osteoporosis. It is also suggested to take Magnesium and vitamin K together for effective results.
Zinc
This nutrient promotes bone growth by helping the body build collagen and absorb calcium properly. Zinc is also important for bone healing. Studies show that high levels of zinc can be found at the sites of bone repair.
Boron
This trace element supports proper bone growth and development by increasing how long vitamin D and estrogen works in the body. Boron also enhances the effect of other nutrients, like calcium and magnesium, and promotes overall hormonal balance. On the other hand, the following nutrients and substances can be damaging to your bones when taken in excess:
Cadmium
This chemical is one reason why many older people suffer from fractures. Cadmium is present in all soils and rocks. It is also added in fertilizers and can be found in some foods – like bread, vegetables and root crops. Consuming cadmium that the body can tolerate is okay. But too much cadmium in the body speeds up the bone loss by increasing bone-eating cells’ formation and activity.
Phosphorus
We need phosphorus for a lot of reasons. It builds bones and teeth, helps form our DNA, filters waste in our kidneys and maintains a regular heartbeat. But having too much phosphorus can be toxic. Phosphorus disrupts our body’s ability to use calcium, magnesium and zinc effectively. It also causes bone loss by taking away calcium from the bones and moving them into the arteries. Carbonated soft drinks spell trouble for older women. This is because they are overloaded with phosphoric acid, a mineral made from phosphorous. Junk foods contain high amounts of it too.
Iron
Iron is the mineral responsible for carrying oxygen in the hemoglobin and transport it across the body so that the body can use the oxygen for different processes. Iron helps take out carbon dioxide as well. But an iron overload in the body might cause osteoporosis by preventing bone mineralization. This means iron may keep osteoblasts from playing their part in good skeletal development.
Caffeine
If you’re obsessed with coffee, better ease up now. More than 4 cups of coffee per day prevents your body from absorbing calcium. According to a study published in the European Journal of Clinical Nutrition, when combined with sugary foods, caffeine has greater negative effects on the bones.
Medical conditions and medications that can cause bone loss:
Bone loss may also be caused by other disorders in the body. Here are several diseases that could increase bone loss:
Hyperthyroidism: Occurs when your thyroid gland produces too much of the hormone thyroxine. Hyperthyroidism can accelerate your body’s metabolism, causing unintentional weight loss and a rapid or irregular heartbeat.
Hyperparathyroidism: A condition in which one or more parathyroid glands become overactive and secrete too much parathyroid hormone (PTH). This causes the levels of calcium in the blood to rise, a condition known as hypercalcemia.
Cushing’s Syndrome: A disorder that occurs when your body makes too much of the hormone cortisol, commonly known as the “stress hormone,” over a long period of time. Autoimmune diseases like rheumatoid arthritis, inflammatory bowel disease and systemic lupus erythematosus affect bone loss. During periods of inflammation, the immune cells release cytokines, an inflammatory chemical that triggers bone loss.
Crohn’s Disease: An inflammatory bowel disease (IBD) that causes inflammation of your digestive tract, leading to abdominal pain, severe diarrhea, fatigue, weight loss and malnutrition.
Celiac Disease: An immune disease in which people can’t eat gluten because it will damage their small intestine. When it comes to medications, long-term use of heparin (a blood thinner), antiseizure medications and oral corticosteroids have been linked to osteoporosis. They can disrupt the bone-rebuilding process.
What happens now?
Sadly, osteoporosis and menopause often go hand in hand. But while menopause is an inevitable part of our life, osteoporosis doesn’t have to be!
Don’t wait until you twist your wrist or (literally) break a leg before taking action. Change your lifestyle, get up, move and eat healthier. There are lots of ways to keep your bones healthy and strong, and it’s not too late to start now.
What changes are you willing to make today? We would love to hear about them so drop them in the comment section below!
Perhaps someone in your family or social circle needs to know about this too! Get the word out by posting this article on your social media profiles. Let them thank you later ?.
Sources:
medicinenet.com/osteoporosis/article.htm#what_are_the_consequences_of_osteoporosis
mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
webmd.com/osteoporosis/features/causes#1
endocrineweb.com/conditions/osteoporosis/risk-factors-osteoporosis
.wallerwellness.com/health-aging/10-ways-to-prevent-or-reverse-osteoporosis
.webmd.com/osteoporosis/guide/bone-mineral-density#1
nof.org/patients/diagnosis-information/bone-density-examtesting/
academic.oup.com/aje/article/185/5/345/2981960
nutritionfacts.org/video/is-milk-good-for-our-bones/
intechopen.com/books/topics-in-osteoporosis/oxidative-stress-and-antioxidants-in-the-risk-of-osteoporosis-role-of-the-antioxidants-lycopene-and-
betterbones.com/bone-health-basics/natures-tips-on-bone-loss-6-signs-and-symptoms-of-bone-health/
onhealth.com/content/1/osteoporosis_in_men
lifespa.com/how-sun-exposure-affects-sleep-and-melatonin-production/
web.archive.org/web/20200929001039/https://www.iofbonehealth.org/national-osteoporosis-society-launches-sunlight-campaign-boost-vitamin-d-levels-summer-months
healthy.net/2005/05/20/how-calcium-and-magnesium-can-slow-down-aging/?cn-reloaded=1
betterbones.com/bone-nutrition/calcium-and-bone/
.eatright.org/food/vitamins-and-supplements/types-of-vitamins-and-nutrients/iron
sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/osteoblast
patient.info/bones-joints-muscles/osteoporosis-leaflet/bisphosphonates
betterbones.com/category/the-natural-approach/
webmd.com/osteoporosis/guide/premenopausal-osteoporosis#1
medicalnewstoday.com/articles/318595#10-cultured-yoghurt
eatthis.com/collagen-rich-foods/
drkarafitzgerald.com/2018/06/08/using-functional-medicine-to-treat-osteoporosis/
mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659#:~:text=Overview,a%20rapid%20or%20irregular%20heartbeat.
my.clevelandclinic.org/health/diseases/14454-hyperparathyroidism#:~:text=What%20is%20hyperparathyroidism%3F-,Hyperparathyroidism%20is%20a%20condition%20in%20which%20one%20or%20more%20of,a%20condition%20known%20as%20hypercalcemia.
niddk.nih.gov/health-information/endocrine-diseases/cushings-syndrome#:~:text=Cushing’s%20syndrome%20is%20a%20disorder,glucose%2C%20also%20called%20blood%20sugar
mayoclinic.org/diseases-conditions/crohns-disease/symptoms-causes/syc-20353304#:~:text=Crohn’s%20disease%20is%20an%20inflammatory,digestive%20tract%20in%20different%20people.
medlineplus.gov/celiacdisease.html#:~:text=Celiac%20disease%20is%20an%20immune,wheat%2C%20rye%2C%20and%20barley.
healthline.com/health/corticosteroids-what-are-they#:~:text=Corticosteroids%20are%20a%20class%20of,asthma
researchgate.net/publication/301712383_The_Relationship_of_Hand_Grip_Strength_with_Bone_Mineral_Density_and_Vitamin_D_in_Postmenopausal_Women
drnorthrup.com/three-drugs-that-i-would-not-take/
therootcauseprotocol.com/iron-toxicity-post-70/
en.wikipedia.org/wiki/Osteogenic_loading
healthline.com/nutrition/the-alkaline-diet-myth#cancer
healthline.com/health/menopause/osteoporosis#osteoporosis-and-menopause
bbc.com/future/article/20181002-how-long-did-ancient-people-live-life-span-versus-longevity
ncbi.nlm.nih.gov/pmc/articles/PMC4534332/#:~:text=Secondary%20osteoporosis%20is%20defined%20as,menopausal%20women%20and%20in%20men.
pubmed.ncbi.nlm.nih.gov/8865143/#:~:text=Abstract,bone%20turnover%20in%20adult%20bone.&text=At%20cellular%20level%20in%20bone,amount%20of%20active%20remodeling%20units.
britannica.com/science/cancellous-bone
spine-health.com/glossary/cortical-bone
happy.guide/2014/11/17/calcium-magnesium/
superhealthychildren.com/vitamin-k2-in-the-raw-vegan-lifestyle/
therootcauseprotocol.com/iron-toxicity-post-70/
👉 What to Do Next
Don’t go just yet — especially if you’ve been feeling off and no one’s given you real answers.
Go to the START HERE page.
It’s where things begin to feel clearer. No more second-guessing, no more sorting through conflicting advice. Just calm, honest support for where you are right now.
And if you haven’t yet, download the FREE GUIDE.
It’s quick, clear, and made to help you feel better — without having to turn your whole life upside down.


Gita is the founder of My Menopause Journey. Since 2014, she has been supporting midlife women by sharing hard-earned learnings from her own experience. To advance her knowledge, Gita puts a lot of her time and effort into understanding the broad spectrum of women’s health. She immerses in extensive research about the physical, mental and emotional aspects of menopause. Gita believes in the life-changing power of healthy, holistic living — this is where she anchors her message to all women. Learn more about her marvelous mission in About us - My Menopause Journey.







most of the people go for various ways to cure this..but after reading this helpful information i would suggest to people to go for this Ayurvedic treatment..no side effect for sure..Thanks for sharing
Hi Amit,
Thanks for sharing your experience about Ayurveda. Come back anytime!
Have a great day!
Gita